Are we ready to mitigate the impacts of COVID-19 on family planning and contraceptives?
Family planning is critical for reducing poverty and ensuring a healthy, productive future for millions of women and girls around the world. But with COVID-19 disrupting health systems, health commodity supply chains, and ways of life in many countries, more and more women and girls are now unable to access the family planning information, products, and services they need. This will have a direct impact on women and girls’ health and well-being for years to come. It will also lead to unwanted pregnancies that could put mothers and children at risk of malnutrition, disease, and economic hardship -- pushing the most vulnerable deeper into poverty.
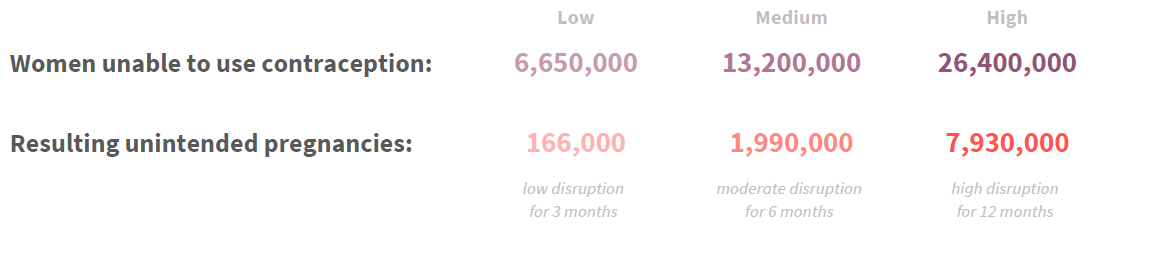
A recent analytical collaboration between the Global Financing Facility (GFF), the Reproductive Health Supplies Coalition, and Avenir Health set out to assess the supply implications of strategies to mitigate the effect of COVID-19 on contraceptive use. Using our new modeling tool, which specifically looks into family planning in the context of COVID-19 our estimates suggest that as many as 26 million women could lose access to family planning in the 36 countries supported by the GFF leading to nearly 8 million unintended pregnancies.
We are already seeing evidence in GFF countries of women and girls being cut off from essential services. For example, in Liberia a combination of supply chain disruptions, mobility restrictions, and fear of COVID-19 are already resulting in a 40% drop in outpatient visits. In fact, according to a recent GFF pulse survey, 8 in 10 GFF countries are reporting declines in demand for essential services, 77% indicate disruptions in the supply of essential health products, and 87% have experienced impacts on the health work force.
The global family planning community has responded swiftly to mitigate these supply and demand shocks with guidance to policymakers. Our modelling collaboration suggests that even with aggressive mitigation measures, COVID-19 could fundamentally change women’s contraceptive use.
Understanding how COVID-19 impacts demand, supply, and equity
A strategy for ensuring access to family planning in the COVID-19 era would first require an understanding of impacts on demand, supply, and equitable access. For example, the desire to reduce face-to-face contact with a health care provider may result in fewer visits for contraceptive methods which require such contact. This might lead to fewer visits for implants, IUDs, and injectables, thereby prompting women and girls to increase use of self-care methods such as pills, condoms, standard days method, patches, and rings, among others. Additionally, many policymakers are increasing the number of product units dispensed during a family planning consultation. This advanced provisioning can reduce contact with the health system but may lead to sharp increases in supply needs in the short-term – a more than three-fold increase in oral contraceptive pills needed over six-months in the GFF countries. Many of these trends would run counter to those pre-COVID-19 which saw heavy reliance on injectables and growing use of long-acting reversible methods. In fact, in 2018, two-thirds of public spending on family planning was on implants and injectables.
Because the private sector delivers 59% of short-term methods in GFF countries, it may prove a more convenient and acceptable source for women to resupply or find bridging methods. However, user fees and the distribution of private facilities may render this option viable only to wealthier women unless subsidies can be used to address affordability. Demand-side financing or public purchasing of services from the private sector are strategies that have proven successful for improving equity in private-sector FP services. Other strategies for ensuring equity may include the use of mobile outreach or community health workers to bring services closer to clients who face restricted mobility or are experiencing declining house-hold income.
Assessing impacts for effective solutions: A tool for policymakers
COVID-19 is fundamentally changing the contraceptive landscape, and by extension, the ability of national programs to meet women’s immediate needs for contraception. The new modeling tool (MICRO) makes it possible to model different scenarios and quantify the impact on shifts in contraception supply and demand. These results can help policymakers develop country-specific mitigation strategies. In contrast to existing models, which look at all methods of contraception and married users, MICRO focuses on modern methods and all users, while taking into account public versus private provision of contraceptives.
The tool is not meant to predict the future but will allow users to explore (and quantify) the potential shifts in contraception needs, as well as the resulting implications of different mitigation strategies and scenarios. Countries may adjust any of the assumptions in the tool to reflect their local market and health system, craft their own responses, and explore service delivery adaptations to meet their changing needs. At the same time, the tool can provide information to donors and program planners to help revisit supply plans and financing models to ensure that contraception is effectively sustained.
Women need more than just products -- they need access to accurate information and proper communication. They also need support emotionally, physically, as well as financially. MICRO is meant to stimulate thinking about comprehensive policy response and service delivery redesign for family planning, thereby supporting decision making by highlighting country specific risks.
We hope that countries can utilize this tool and data to dig into what is best for their communities and to implement mitigation strategies that maintain essential reproductive health services for women and girls.
A longer commentary has recently been published in Global Health Science and Practice