Nigeria
CASE STUDY
Nigeria
As a lower-middle-income country with a large, rapidly growing population, Nigeria is facing considerable pressure on how it provides and pays for health services for its people. Nigeria, which joined the GFF in 2015, has among the lowest per capita health expenditures in the world and spends less on health than other countries with comparable income levels. At the same time, the Boko Haram insurgency has left the country’s North East region a particularly fragile area, curtailing service delivery, destroying health infrastructure, and leaving households with limited access to health and nutrition services. This period of social and political unrest and division has hindered efforts to address poverty and inequality.
In an effort to increase funding for health and deliver a universal Basic Minimum Package of Health Services (BMPHS) to all Nigerians, the federal government established the Basic Health Care Provision Fund (BHCPF). To accelerate the focus on the nation’s poorest and most vulnerable populations, and in alignment with the investment case, the Nigeria State Health Investment Project (NSHIP) has been expanded into the conflict-affected Northern regions of the country. Though it is not possible to attribute results to any one entity, intervention, or health reform, data from a recent Demographic and Health Survey (DHS, 2018) are indicative of progress in several key reproductive, maternal, neonatal, child, and adolescent health and nutrition (RMNCAH-N) indicators, including in the Northern regions where the NSHIP has been scaled up. However, these results also highlight remaining gaps in service delivery, quality, and access, alongside a concerning nutrition situation that continues to exist and is particularly serious in the Northern regions of the country. The continued scale-up of the NSHIP, as well as the government’s introduction of the Accelerating Nutrition Results in Nigeria (ANRIN) project, will support further expansion of the BMPHS while addressing the nutritional needs of mothers and children in the country’s most vulnerable regions.
Trends in key RMNCAH-N indicators (2008-2013, DHS)
- Maternal mortality ratio:
Rose from 545 to 576 per 100,000 live births - Under-five mortality rate:
Rose from 38 to 120 per 1,000 live births - Neonatal mortality rate:
Declined from 40 to 37 per 1,000 live births - + Stunting prevalence among children under five:
Rose from 34.3 to 44 percent - Wasting prevalence among children under five:
Rose from 10.8 to 11 percent - Age-specific fertility rate for adolescents (15-19 yrs):
Declined from 126 to 122 per 1,000 live births
Country Priorities:
The National Health Act
The National Health Act served as a significant catalyst for domestic resource mobilization in Nigeria, triggering an initial allocation of domestic resources for geographically and programmatically prioritized work on key health and nutrition services. The National Health Act was signed into law in 2014, pledging that all Nigerians were entitled to a free, universal Basic Minimum Package of Health Services (BMPHS). This package of high-impact services includes the equitable provision of family planning, antenatal care, facility-based delivery, screening for non-communicable diseases, malaria prevention and treatment, and prevention of and treatment of illnesses affecting children under 5.
To accelerate progress in achieving these outcomes, the GFF partnership has supported the Government of Nigeria to: (i) increase the overall funding envelope for the implementation of the National Health Act and improve the efficiency with which these funds are used; and (ii) reach the nation’s poorest and most vulnerable populations, through the expansion of the NSHIP into the conflict-affected North East of the country, where historically it has been extremely difficult to provide services.
Increasing the allocation
and efficient use of funds for the operationalization of the National Health Act and Basic Minimum Package of Health Services
The principal funding vehicle for the BMPHS is the Basic Health Care Provision Fund (BHCPF), which is being introduced in all 36 states and the Federal Capital Territory of Abuja, as a mechanism to channel increased domestic and international financing. In 2018, the GFF and the Bill and Melinda Gates Foundation, with technical assistance from partners including the World Bank and USAID, provided funding to the BHCPF to test the proof of concept. In addition, the GFF partnership motivated the government of Nigeria to pledge US$180 million (1% of the annual federal budget) in domestic resources to support the BHCPF annually. A first allocation from the government budget was made in 2018.
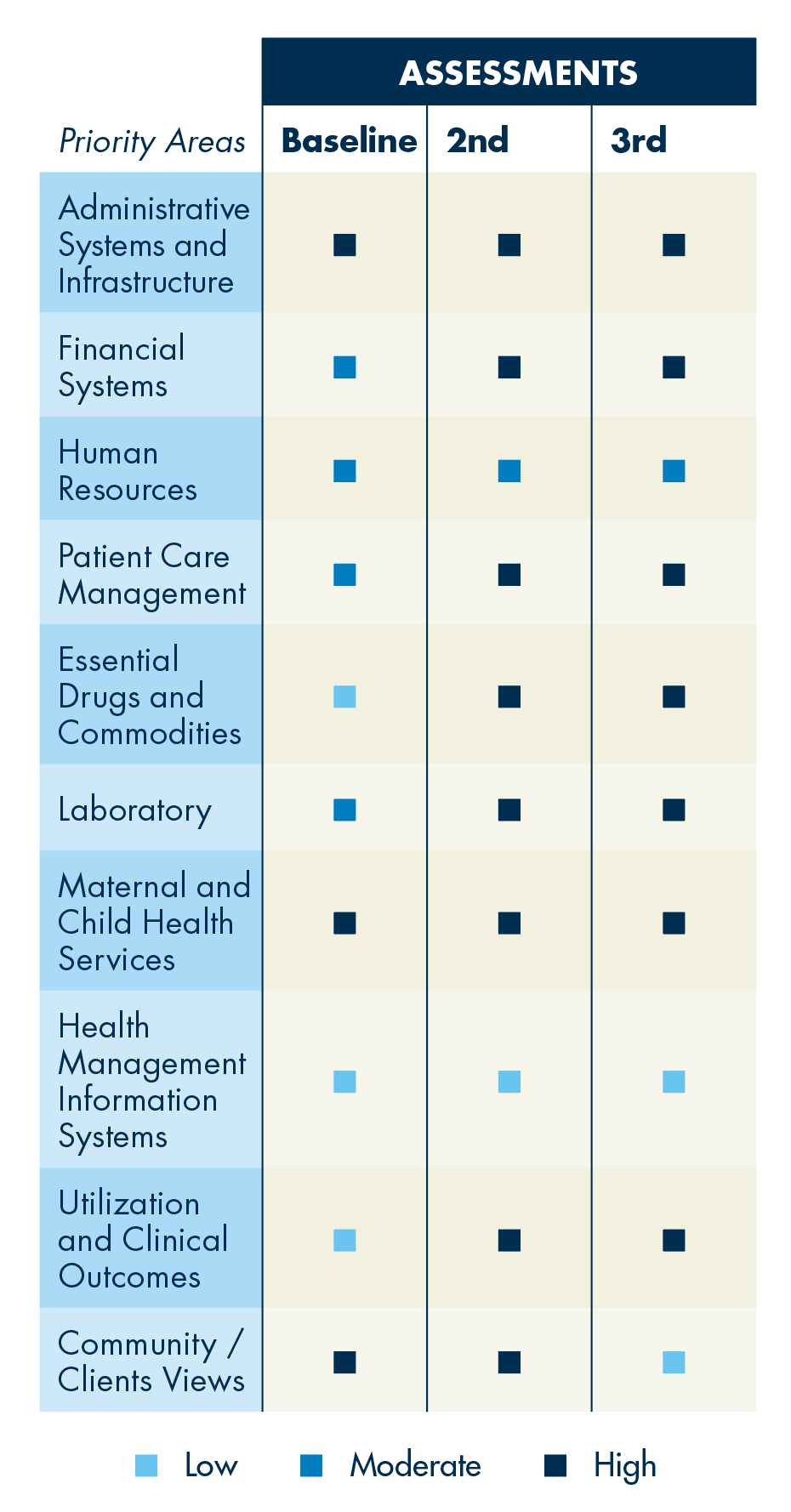
The BHCPF includes an accreditation system to strengthen the monitoring of quality of care and clinical governance. A scorecard system is used to monitor performance in 10 priority areas (Figure 1), with additional oversight from the governance and accountability secretariat, which will conduct periodic assessments to determine compliance and effectiveness. The quality scorecard allows the BHCPF to focus on results and uses an electronic reimbursement technology for each facility.
To improve the efficiency of funds allocated to the operationalization of the BMPHS, the Government of Nigeria, with support from the GFF, conducted a preliminary resource mapping to improve alignment of external financing. This exercise was an important step in determining where and how external financing was to be budgeted, as well as to elicit areas of duplication and gaps in financing and activities.1 The resource mapping highlighted that the investment case remains underfunded (58 percent gap in financing), and that efforts need to be made to bring additional funding aligned around the BHCPF. This resource mapping will be repeated on an annual basis; a more detailed subnational resource mapping will be completed
by early 2020.
Rebuilding the health system
in the conflict-affected North East through the expansion of the Nigeria State Health Investment Project
The GFF is a co-financier of the NSHIP, a program that brings new attention to critical issues such as chronic malnutrition. The NSHIP uses a performance-based financing approach that creates incentives to improve maternal and child health outcomes. In other words, financing is provided to preselected public and private primary health care centers directly, based on facilities’ achievement of pre-agreed results on health outcomes. Decision-making is also decentralized to the facility level, giving facilities more autonomy and flexibility to innovate and adopt their own locally focused solutions to achieve results.
Results
In the conflict-affected region supported by NSHIP and other partners, several achievements were recorded in 2018, both in increasing access and use of health care services and in strengthening health systems. Services financed by NSHIP were expanded to 39 local government agencies serving 13.3 million people. In these areas, 38 secondary health care facilities and 437 primary health care facilities were revitalized, including both infrastructure and human resource improvements. Likely driven by such improvements, an additional 43,000 women received antenatal services and an additional 51,000 deliveries were attended by a skilled birth attendant, with an overall increase in deliveries assisted by a skilled birth attendant from 60 percent in 2017 to 70 percent in 2018. An additional 40,000 children under the age of 1 year were immunized, with vaccine coverage (DPT3) increasing from 34 percent in 2017 to 48 percent in 2018.
Because the implementation of the BHCPF (2018) is so recent and the development of systems to collect and report data on RMNCAH-N indicators is ongoing, data are not yet available on improvements in quality, clinical governance of service delivery, and RMNCAH-N outcomes specifically attributable to the BHCPF roll-out. Despite the inability to attribute results to any one entity, intervention, or health reform, data from a recent Demographic and Health Survey (DHS, 2018) indicate progress on several key RMNCAH-N indicators, including in the Northern regions where the NSHIP has been scaled up, as described above. Improvements in the coverage and quality of maternal and child services included in the BMPHS have been seen at both national and regional levels. This includes, for example, improvements in the percentage of women benefitting from deliveries assisted by a skilled birth attendant, postnatal consultations, use of insecticide treated nets (ITN) and intermittent preventive treatment, and reductions in child wasting.
While key RMNCAH-N indicators in the North East and North West regions lag well below national levels, the rate of improvement seen in these regions over time is in several cases well above national level improvements. For example, for the 2008–2018 period, skilled birth attendance rose by 11.2 percentage points (from 16.5 to 27.7 percent) in the North East and by 8.3 percentage points (from 10.7 to 19 percent) in the North West (Figure 2).
Figure 2
Rate of skilled birth attendance in Nigeria, nationwide and northern regions, 2008, 2013, and 2018
The percent of skilled birth attendance in the Northern regions of Nigeria is lower than the national average, but improvements there over the last decade far surpass those seen at the national level
The percentage of women receiving postnatal consultations within 2 days after giving birth also showed gains at the national level. Between 2013 and 2018, among women who gave birth in the two years preceding the survey, the proportion who had their first postnatal consultation rose from 39.6 to 41.8 percent nationally (a 6 percent increase), with improvements in the North East and North West rates representing increases of 6 and 23.5 percent, respectively (Figure 3).
Figure 3
Postnatal consultation within 1-2 days of birth in Nigeria, nationwide and northern regions, 2013 and 2018
The percentage of women receiving postnatal consultations increased over the last 5 years, with increases in the Northern regions equivalent to or greater than those seen at the national level
Drastic improvements in malaria prevention, a key intervention under the BMPHS and at the core of funding provided by external partners such as the Global Fund and the World Bank, have also been observed in Nigeria over time. This is reflected in large increases in bed net use among both children and women (Figure 4), as well as in the delivery of intermittent preventive treatment (IPT) during antenatal care (Figure 5). Trends in bed net use are similar for children and women, as well as in Northern regions compared to national trends. Drops in bed net usage are observed in 2013, but 2018 data show an impressive recovery, with coverage rates far exceeding both 2013 and 2008 numbers.
Figure 4
Use of treated mosquito nets among children under 5 and pregnant women in Nigeria, nationwide and northern regions, 2008, 2013, and 2018
Drastic increases in bed net usage were observed at both national and regional levels in Nigeria, especially from 2013-2018
Figure 5
Percentage of women (ages 15-49) with live births who during pregnancy took two or more doses of IPT, nationwide and northern regions, 2008, 2013, and 2018
National and regional increases in the coverage of IPT2+ and IPT3+ signal important improvements in the quality of service delivery in Nigeria over time
The national and regional increases in the proportion of women who had access to two and three or more doses of IPT (IPT 2+ and IPT3+) have been dramatic, signaling a trend in improvements in the quality of antenatal care services. These trends were observed both at national and regional levels, with the Northern regions exhibiting improvements that were equal to or greater than those seen at the national level. For example, nationwide IPT 2+ coverage increased eight-fold (from 4.9 to 40.4 percent), while in the North East and North West, the increase in this coverage was 14-fold (from 2.9 to 40.7 percent) and 8-fold (from 3.9 to 34.1 percent), respectively.
Progress on nutrition indicators in Nigeria has been mixed (Figure 6). Significant improvements in the proportion of children suffering from wasting were observed in the last decade, likely contributing to reductions in child mortality given the close linkages between wasting and mortality. In both of the Northern regions, wasting was reduced by half or more, from 22.2 percent in 2008 to 10.1 percent in 2018 in the North East, and from 19.9 percent in 2008 to 10.1 percent in 2018 in the North West. These trends reflect significant funding provided for the treatment of severe acute malnutrition in recent years. Alongside these impressive reductions in wasting, however, were increases in the prevalence of stunting, including in Northern regions of the country. This indicates—as recognized by the Government of Nigeria through its ANRIN project—the need to go beyond financing the “nutrition emergency” (i.e., severe acute malnutrition), to address the “nutrition crisis” (i.e., child stunting, maternal malnutrition, and micronutrient deficiencies) that affects far larger numbers of women and children.
Conclusion and
Work Going Forward
With the expansion of the NSHIP into Northern, conflict-affected regions of the country, results from the 2018 DHS survey demonstrate that significant progress has been made in improving key RMNCAH-N outcomes. However, these results also highlight remaining gaps in service delivery, quality, and access, alongside a continuing nutrition situation that is of concern. Looking forward, and in order to accelerate the reduction of child stunting—which is a priority under the National Health Act—the Government of Nigeria, together with the World Bank, GFF, and other technical partners, will implement the ANRIN project. This US$232 million project is co-financed by the GFF and IDA, and benefits from a technical assistance pooling mechanism funded by the Power of Nutrition, the Aliko Dangote Foundation, and the Bill and Melinda Gates Foundation. The project is geographically centered on the 12 states, in all regions of the country, where the prevalence of stunting is the highest, and it will use a results-based contracting approach that leverages the capacity of non-state actors. The project will address the nutritional needs of mothers and children, with a special emphasis on the nutritional needs of adolescent girls and their children.