The Global Financing
Facility for Women,
Children and Adolescents
Annual Report 2018-2019
Letter from the Director
This has been a landmark year for global health. At various international conferences, world leaders and advocates reaffirmed their commitments to ending the preventable deaths of women, children, and adolescents by 2030, achieving universal health coverage (UHC) by strengthening primary health care, and closing the enormous global financing gap to achieve health and well-being for all.
For the Global Financing Facility for Women, Children and Adolescents (GFF), the past year was marked by two exciting milestones in our mission to expand the delivery of quality, affordable health care to the most vulnerable people around the globe. In November 2018, thanks to generous support from the governments of Burkina Faso, Canada, Cote D’Ivoire, Denmark, Germany, Japan, The Netherlands, Norway, Qatar, and the United Kingdom, as well as the Bill and Melinda Gates Foundation, the European Commission, Laerdal Global Health, and the Susan T. Buffet Foundation, the world pledged US$1 billion in additional funding for the GFF Multi-Donor Trust Fund. With this increased capacity, in May 2019 the GFF announced that it has enlarged its reach to an additional nine countries, bringing the total number of countries supported by the GFF partnership to 36.
This ability to extend the GFF’s impact is more urgent than ever. The countries supported by the partnership—one-third of which are classified as fragile and conflict-affected states—experience many of the world’s most pressing challenges in sexual and reproductive health, and they have the poorest outcomes in maternal, newborn, child, and adolescent health and nutrition. The latest data from the World Bank and the World Health Organization show that without significant changes in health financing for these countries, even by the year 2030 UHC will remain out of reach for billions of people.
Addressing these challenges starts with strong country leadership. GFF partner countries share a commitment to put women, children, and adolescents at the forefront of their health reform efforts and to invest in smart, sustainable health systems to ensure that no one is left behind. This report showcases how GFF-supported countries are taking ownership of their development, financing, and results agendas and are leading the way to close their health financing gaps.
In the four years since its founding, the GFF partnership has started on the path to transform development assistance for health by aligning external resources with domestic financing and linking these resources to proven performance in improving women’s, children’s and adolescent health. Five core elements of the GFF partnership have contributed to our early results:
- Country-led: GFF partners—governments, donors, technical partners, civil society and the private sector—are coming together to support government-led investment cases that prioritize the use of available resources and high-impact health services to benefit the poorest and most vulnerable communities.
- Alignment: By aligning external funding around a country-led, country-owned plan, the GFF approach enables all partners to make more cost-effective and efficient investment decisions in health and nutrition. Decisions on priorities and funding are being made using rigorous data, with a focus on quality and the achievement of results. In many GFF-supported countries, funds are triggered when agreed upon targets on quality, access, or domestic resource disbursements are achieved.
- Evidence-driven: The GFF approach promotes smarter decision-making and better health outcomes, using the most rigorous data and linking payments to achieving agreed targets.
- Leverage: By catalyzing innovative financing mechanisms—such as development impact bonds and the linking of GFF Trust Fund grants to concessional financing through the World Bank’s International Development Association (IDA)—the GFF is multiplying available resources for women’s, children’s, and adolescent health and is enabling countries to strengthen their health systems on a national scale.
- PHC to UHC: Through their national platforms, countries are translating their visions of UHC into practice, with a focus on building well-functioning, integrated primary health care (PHC) systems that provide the necessary foundation to accelerate progress toward quality, affordable care for all.
Although the GFF partnership is still very young, I am convinced that if we stay focused on these five pillars, we will see continued progress in health equity toward our goal to give all women, children, and adolescents the opportunity to live healthy, productive lives.
I am honored to work with our many GFF partners around the globe in governments, civil society, international organizations, philanthropy, and business who share our commitment to this mission. This report shows what’s possible when all these partners come together to prioritize quality, sustainable results and empower countries and their citizens to lead.
Muhammad Pate
Director, Global Financing Facility
OVERVIEW
Big Year, Bigger Challenges
Despite the significant recent progress in global health and development outcomes, equitable access to affordable, quality health care still remains out of reach for nearly half the world’s population. Paying for the care they need causes financial hardship for more than 935 million people and pushes nearly 90 million people into extreme poverty every year. If current trends continue, up to 5 billion people will remain unable to access essential health care as of 2030—the deadline that world leaders have set for achieving universal health coverage (UHC) and the Sustainable Development Goals (SDGs). These are the stark messages of the 2019 Global Monitoring Report, which calls for countries to increase their investments in primary health care (PHC) as the pathway to achieving UHC.
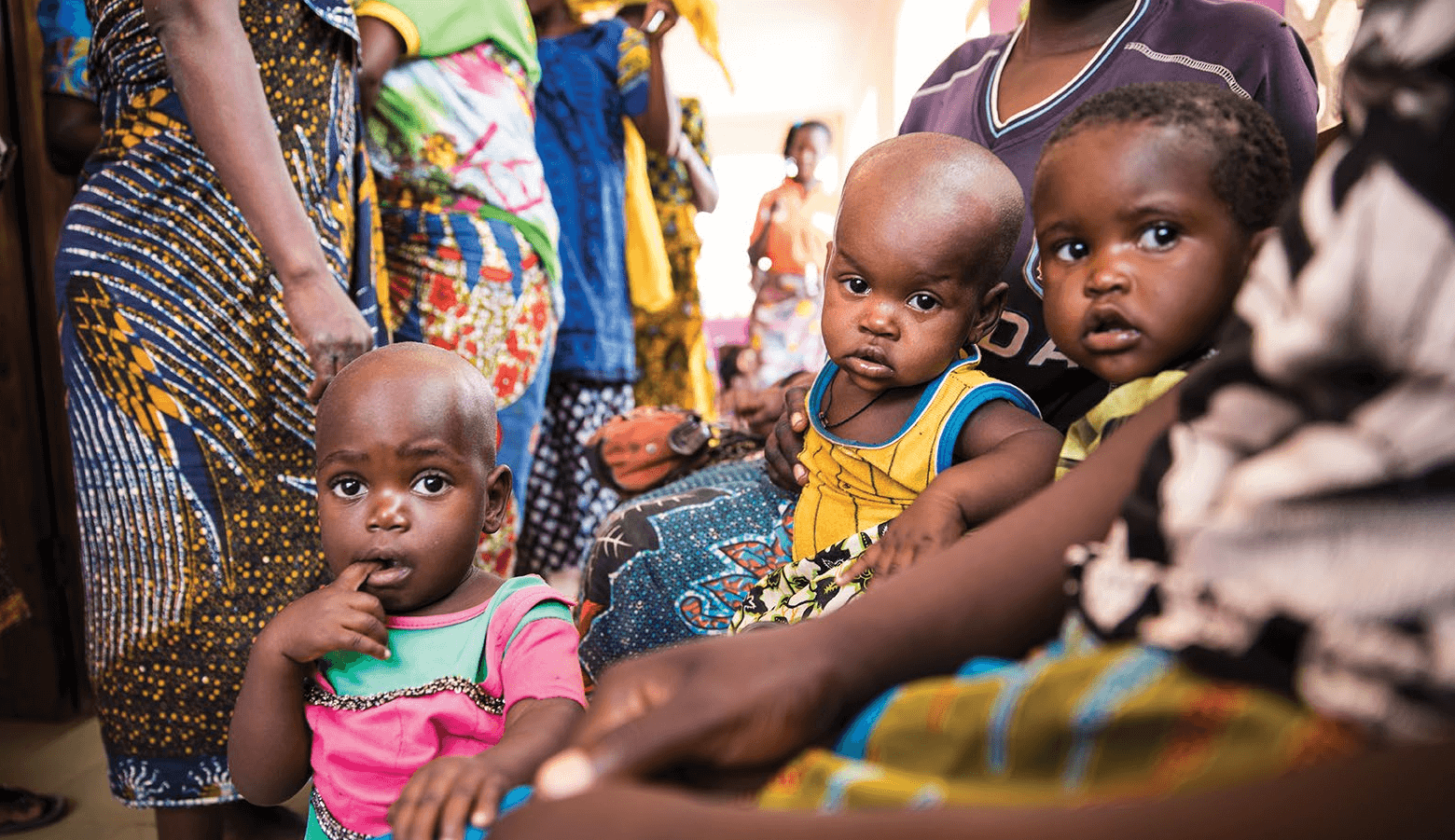
Quite simply, this is an urgent matter of life and death for women, children, and adolescents, who are most affected by the continuing lack of access to quality, affordable primary health care.
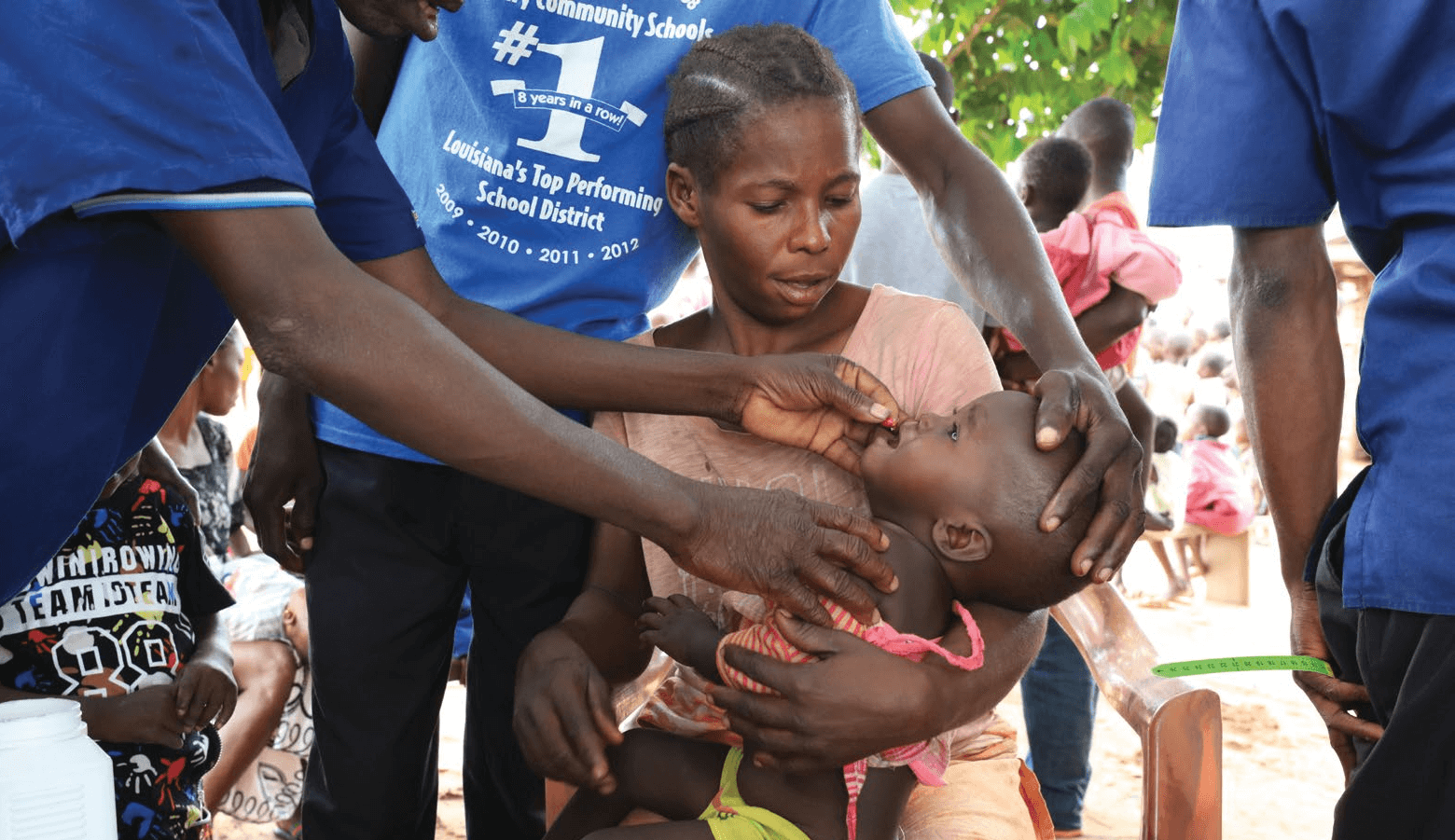
An estimated 6.2 million children and adolescents under age 15 died in 2019, and more than 290,000 women died due to complications during pregnancy or childbirth in 2017. The latest estimates show that 2.8 million pregnant women and newborns die every year—one every 11 seconds—mostly of preventable causes.2 Hundreds of millions more are at high risk of not getting the health and nutrition they need to thrive, particularly in regions mired in instability and conflict.
Yet in most low and lower-middle income countries today, health financing is too low, too inefficient, and too inequitable to address these challenges.
Spending on health care from all sources averages just US$40 per capita in low-income countries and US$135 per capita in lower-middle-income countries, as compared with spending of US$455 per capita in upper-middle-income countries and more than US$3,100 per capita in high-income countries. The World Bank estimates that 54 low-income and lower-middle-income countries will need an additional US$176 billion by 2030 to finance an essential package of quality services for all.
This is where the Global Financing Facility for Women, Children and Adolescents (GFF) partnership comes in: To help the poorest countries close their health financing gaps and improve the health and nutrition of women, children, and adolescents.
In only its fourth year, as of 2019 the GFF has expanded its support to 36 countries, a ninefold expansion from the 4 countries the GFF supported when it was established in 2015.4 This growth was spurred by a strong expression of demand for the GFF country-led approach, which aligns resources from international partners and links them to domestic health plans and budgets to drive better results.
The most recent growth in the GFF’s work was made possible
by more than US$1 billion in pledges of additional financing over the past year for the GFF
Trust Fund.
This included continuing generous support from the GFF’s early champions, including the Bill & Melinda Gates Foundation, the governments of Canada, Norway, and the United Kingdom, and MSD for Mothers, as well as support from 10 new donors in 2018-19.5 Reaching these two milestones, GFF is well on the way to achieving its goal of supporting the 50 countries with the world’s highest maternal and child mortality burdens and financing needs.
While results vary widely from country to country, the GFF’s country-led and partnership-driven approach is already reaping dividends for the health of millions of poor and vulnerable women, children, and adolescents in several ways:
- Increasing domestic resource use and mobilization: Per-capita health expenditure financed by domestic sources has increased in 19 of the 27 GFF countries highlighted in this report, according to the most recent available data. The impact of these increases is translating into more resources for underserved communities across these nations. For example, in Kenya all 47 counties met the criteria of increased allocations to health in their budgets over the past two years, with some allocating more than 30 percent of their budget to health (well above the 20 percent requirement). Nineteen of the 47 counties in Kenya increased their budget allocations for health by at least 5 percent.
- Improving health outcomes: The most recent data available show that neonatal and under-five mortality have decreased in 27 countries receiving GFF support, and the adolescent fertility rate has decreased in 26 of them. These outcomes are the result of expanding the delivery of lifesaving health care for women, children, and adolescents. In Tanzania, for example, antenatal care improved from an average of 35.8 percent of pregnant women in 2014 to 64.1 percent in 2018, with almost one-third of Tanzania’s regions reaching 70 percent or more of pregnant women. Alongside these improvements in care in Tanzania were increases in the regional average for the share of births at a health facility, which rose from 67.0 percent in 2014 to 79.6 percent in 2018.6
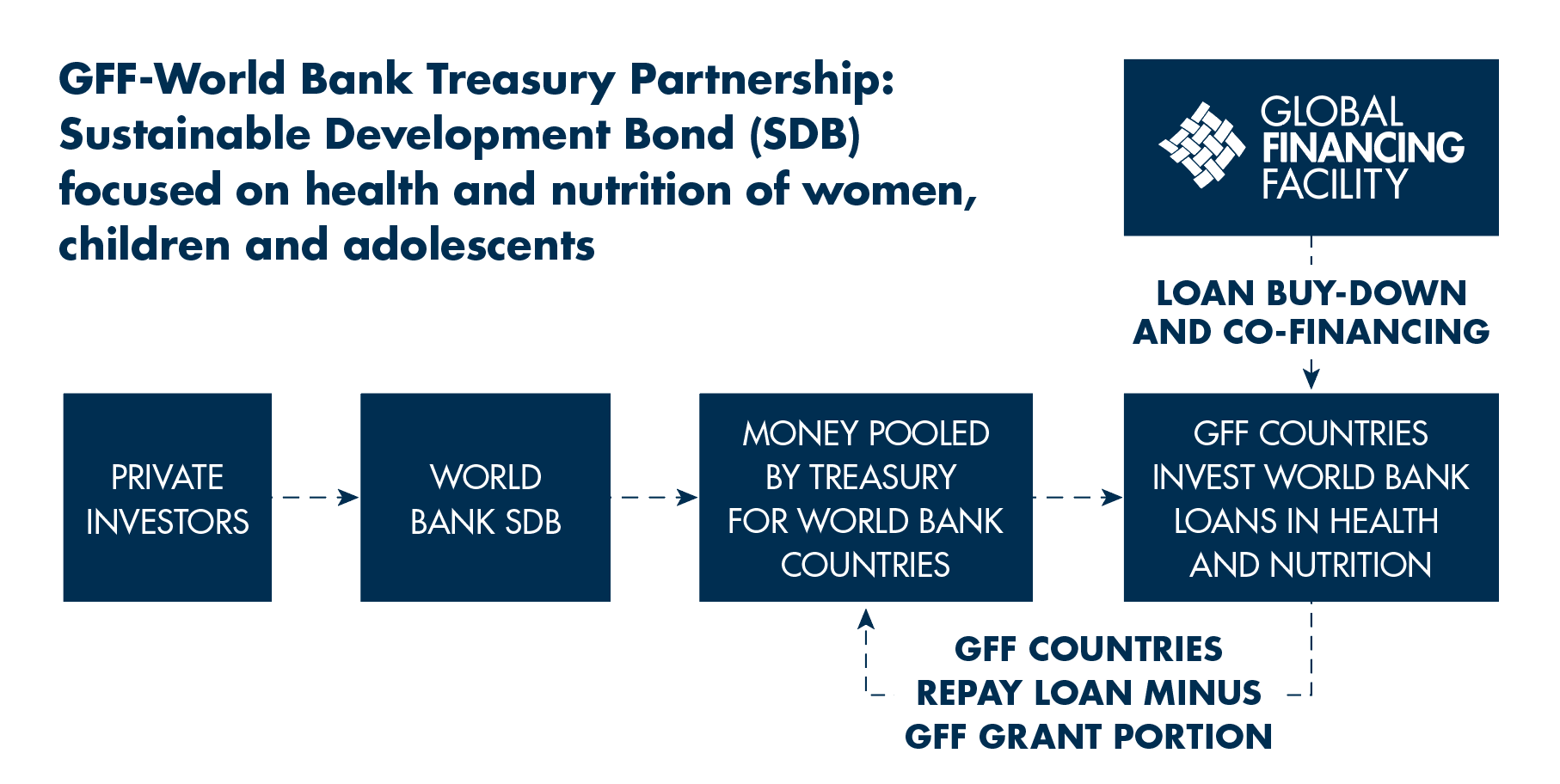
- Catalyzing innovative financing: The GFF has helped mobilize more than US$2 billion in private capital to date, deploying a range of innovative financing tools. In partnership with World Bank Treasury, the GFF supported a Sustainable Development Bond series focused on the health and nutrition of women and children. The GFF Trust Fund’s co-financing and loan buy-down grants make this financing more accessible to GFF countries. In 2019, the GFF worked with Grand Challenges Canada, the World Bank, and other partners to launch a groundbreaking Development Impact Bond focused on newborn health in Cameroon, which seeks to save the lives of at least 2,200 infants each year by expanding the use of Kangaroo Mother Care.
50 countries are eligible for GFF financing; to date, 36 countries are receiving GFF support.
Download results for select countries:
Case Studies
CASE STUDY
Democratic Republic
of the Congo
The Democratic Republic of the Congo (DRC) is home to vast natural resources, but it is
also one of the world’s poorest countries, severely limiting its ability to improve health care
systems. For years, the country endured armed conflict, political instability, and outbreaks
of hemorrhagic disease—most recently an Ebola virus epidemic that is the second-worst
ever recorded worldwide.
READ CASE STUDY
CASE STUDY
Ethiopia
One of the first countries to join the GFF—in 2015—Ethiopia has made substantial
progress in reducing under-five mortality, maternal deaths, and adolescent fertility. These
achievements are impressive, but the Government of Ethiopia recognizes that continued
efforts are needed to strengthen the nation’s health system to achieve the objectives of its
investment case. That investment case, called the Health Sector Transformation Plan, aims
to increase the equitable coverage of, access to, and use of essential health services.
READ CASE STUDY
CASE STUDY
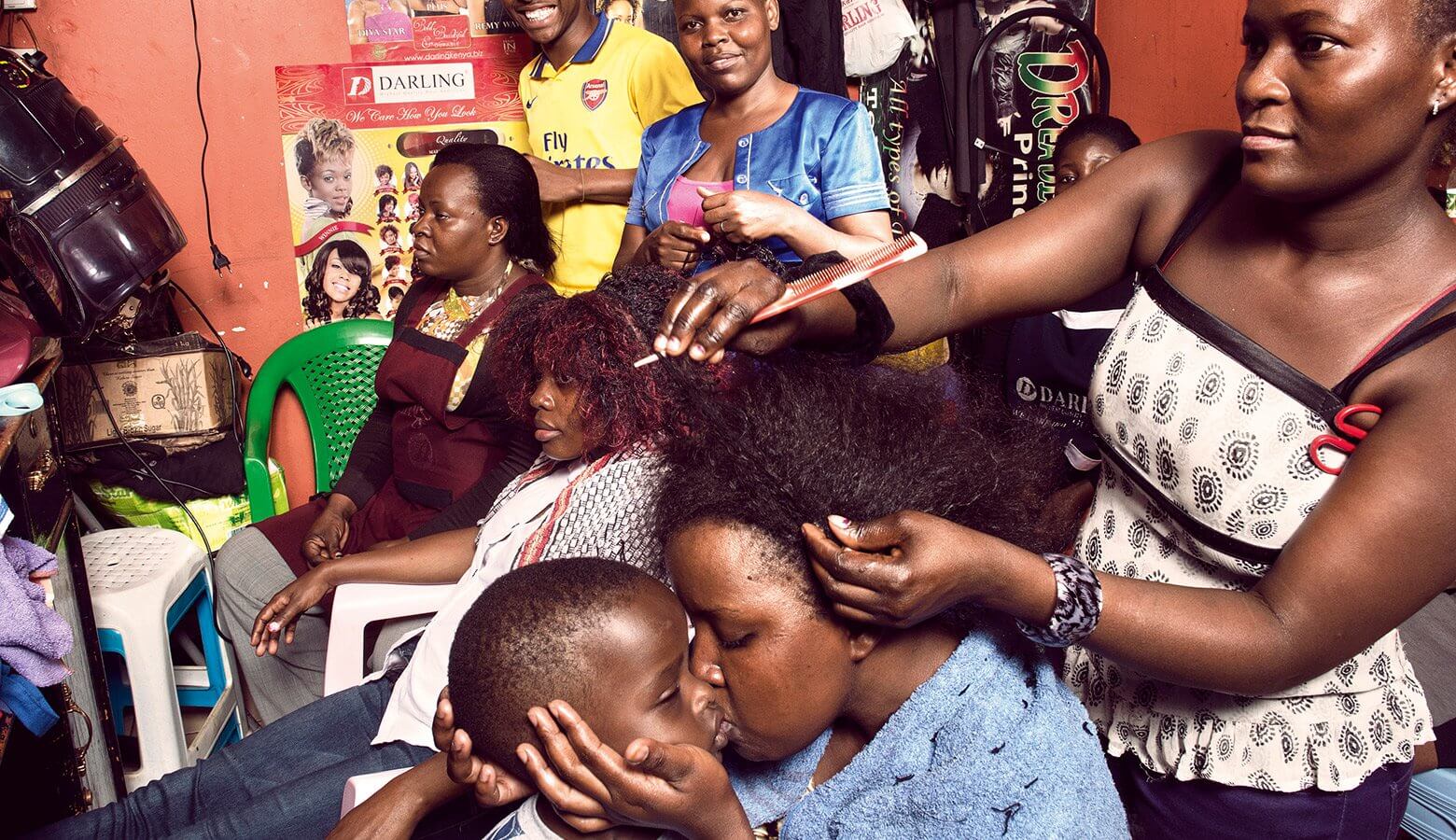
Kenya
Kenya has made substantial advances in reducing maternal and child deaths since the late
1990s. The country is continuing to tackle maternal and child mortality through several
financing and programmatic mechanisms, all of which are aligned with the priorities laid
out in Kenya’s Health Sector Strategic Plan (KHSSP) and Investment Framework.
READ CASE STUDY
CASE STUDY
Mozambique
Since its civil war ended in 1992, Mozambique has achieved substantial reductions in maternal, under-five, and neonatal mortality rates. However, progress in these areas has been uneven and limited for people in the poorest income quintiles and for rural populations. Under the leadership of the Government of Mozambique and in collaboration with a range of partners, including the GFF, a five-year investment case was developed.
READ CASE STUDY
CASE STUDY
Nigeria
As a lower-middle-income country with a large, rapidly growing population, Nigeria is facing considerable pressure on how it provides and pays for health services for its people. Nigeria, which joined the GFF in 2015, has among the lowest per capita health expenditures in the world and spends less on health than other countries with comparable income levels.
READ CASE STUDY
CASE STUDY
Tanzania
Tanzania recorded major improvements in several RMNCAH-N outcomes in the decade between 2005 and 2015. At the same time, progress on some indicators has been mixed, with significant regional variations. Tanzania’s commitment to improving maternal, newborn, child, and adolescent health and nutrition (RMNCAH-N) outcomes is evidenced by the country’s commitment to join the GFF.
READ CASE STUDY
CASE STUDY
Uganda
Uganda has achieved steady improvements on several key maternal and child health indicators over the past 20 years (Box 1). However, significant challenges remain, and public expenditure on health remains low, at just 7 percent of the national budget, equivalent to US$14 per capita, according to the Uganda National Health Financing Strategy 2016.
READ CASE STUDY
Strengthening Civil Registration and Vital Statistics to Protect Women, Children, and Adolescents
Civil registration and vital statistics (CRVS) systems in most GFF-supported countries are weak, with only Guatemala having a fully functional electronic CRVS system to provide basic demographic and health data. In 20 of the 27 GFF-supported countries highlighted in this report, less than 80 percent of children under the age of five are registered with civil registration authorities. Fourteen countries have no information on death registration, and 24 have no information on the cause of death. Lack of these statistics undermines the basic human rights of women, children, and adolescents and has a negative impact on the availability of data at the national and subnational levels that are required for planning and monitoring of health outcomes.
Percentage of Children under the Age of Five Registered with National Civil Registration Authorities in GFF-Supported Countries

Financials
As of June 30, 2019, contributions to the GFF Trust Fund total US$992.8 million equivalent, of which $629 million is committed for 33 projects in 27 countries and is combined with an additional $4.8 billion IDA/IBRD. Seventy-eight percent of the funding supports GFF countries in Africa, followed by 10 percent in South Asia, 9 percent in East Asia, and 3 percent in Latin America and the Caribbean (Figure 1). GFF-supported projects in 23 countries have been approved by the World Bank Board of Executive Directors. Fifteen countries are implementing GFF-World Bank financed projects, with a total of US$1.02 billion disbursed by these projects, of which US$120 million is from the GFF Trust Fund and US$901.5 million is from IDA/IBRD. The full list of Board-approved projects is provided in Table 1.
Share of GFF Portfolio by Region

Table 1 List of Board Approved Projects as of June 30, 2019
| Project | GFF amount | IDA amount | IBRD |
|---|---|---|---|
| Tanzania | $40 | $200 | |
| DRC (AF-CRVS) | $10 | $30 | |
| Cameroon | $27 | $100 | |
| Nigeria (AF) | $20 | $125 | |
| Kenya | $40 | $150 | |
| Uganda | $30 | $110 | |
| Liberia (AF) | $16 | $50 | |
| Guatemala | $9 | $100 | |
| DRC (AF) | $40 | $320 | |
| Ethiopia | $60 | $150 | |
| Bangladesh | $15 | $500 | |
| Bangladesh - Education | $10 | $510 | |
| Mozambique | $25 | $80 | |
| Rwanda (Health) | $10 | $25 | |
| Afghanistan | $35 | $140 | |
| Rwanda (SP-AF) | $8 | $80 | |
| Guinea | $10 | $45 | |
| Indonesia | $20 | $400 | |
| Nigeria (Nutrition) | $7 | $225 | |
| Burkina Faso | $20 | $80 | |
| Nigeria (Part 2) | $20 | $0 | |
| CAR | $10 | $43 | |
| Malawi | $10 | $50 | |
| Mali | $10 | $50 | |
| Cote d'Ivoire | $20 | $200 | |
| Cambodia | $10 | $15 | |
| Haiti | $15 | $55 | |
| DRC Nutrition | $10 | $492 | |
| Vietnam | $17 | $80 |
Share by: