Kenya
CASE STUDY
Kenya
Kenya has made substantial advances in reducing maternal and child deaths since the late 1990s. The country is continuing to tackle maternal and child mortality through several financing and programmatic mechanisms, all of which are aligned with the priorities laid out in Kenya’s Health Sector Strategic Plan (KHSSP) and Investment Framework. To assist in putting this Investment Framework into action, the GFF partnership and key donors are working with national and county governments to support both financing and technical assistance activities aimed at strengthening improvements in health service quality, alignment, financing, and implementation.
In the last two years, progress has been made both in improving financing and in expanding services: All 47 counties in Kenya have increased allocations to health in their budgets, and the coverage of antenatal care, skilled birth attendance, and family planning has increased. This is especially impressive given the significant disruptions faced by the health sector in 2017 due to nurse and doctor strikes, which lasted close to a year and contributed to deteriorations in most health service delivery indicators. At the same time, despite improvements since 2017, progress remains mixed across counties and for certain indicators, such as the coverage of child immunizations. Continued support to strengthen county-level shifts in planning, budgeting, and data use will be critical to better targeting health services and achieving the goals of the KHSSP.
Trends in key RMNCAH-N indicators (1998–2014)
- Maternal mortality ratio:Declined from 590 to 362 per 100,000 live births
- Under-five mortality rate:Declined from 111 to 52 deaths per 1,000 live births
- Share of women who had another child less than 24 months after their previous child:Declined from 23.1 to 17.9 percent
Country Priorities: The Reproductive, Maternal, Newborn, Child and Adolescent Health (RMNCAH) Investment Framework
In early 2013, the Government of Kenya enacted a process of devolution, which included the transfer of planning and budgeting functions to county governments. This is why, in 2015 when Kenya became a GFF-supported country, the decision was made to create an Investment Framework that would provide general guidance to counties on relevant health areas. Specifically, the framework would guide counties on where to focus their health financing and service delivery in order to achieve national-level goals in reproductive, maternal, newborn, child, and adolescent health and nutrition (RMNCAH-N). This Investment Framework is therefore closely aligned with the KHSSP.
Given the decentralization of health planning and budgetary functions in Kenya, the Investment Framework is put into effect at the county level through annual workplans. These workplans are county-specific, and they are monitored using an RMNCAH-N scorecard that tracks KHSSP indicators pulled monthly from the routine monitoring system (DHIS2). On a quarterly basis, counties review and discuss scorecard outcomes and agree on specific activities to drive course correction through an action tracker that is linked to the scorecard.
To support quality improvements, alignment, financing, and implementation of annual county work plans, various partners, including the GFF partnership, have provided both financing and technical assistance. Two main vehicles are used to channel this support: (1) the Transforming Health Systems for Universal Care Project, which uses a results-based approach; and (2) the RMNCAH Technical Assistance Multi-Donor Trust Fund (MDTF).
Support to the Transforming Health Systems for Universal Care Project
By tying funding directly to performance, the Transforming Health Systems for Universal Care Project (THS-UCP), cofinanced by the World Bank and the GFF Trust Fund, is encouraging county governments to shift from a health-inputs model to a health-results model. In Kenya, county governments are primarily responsible for planning and budgeting for health service delivery. Every year,
they receive funding that is tied directly to their performance on four indicators: coverage of antenatal care services, skilled birth attendance, child immunization, and use of modern contraceptives. This creates an incentive to prioritize both the delivery and the utilization of these essential
health services.
Other focus areas of the THS-UCP, which aim at the overall objective of helping the Kenyan government achieve universal health coverage (UHC) by 2022, are health financing reforms and improved mobilization and use of domestic resources. First, to stimulate greater mobilization and use of domestic resources at the county level, the THS-UCP project’s eligibility criteria include a requirement that county governments allocate at least 20 percent of their budgets to health and that this percentage be increased over the previous year’s allocation if a county had allocated less than 30 percent of their budget to health. Second, the government has begun implementing Phase I of UHC in four counties, using a supply-side financing approach. By removing out-of-pocket payments for hospital-based services, the goal is to increase the use of hospital health services while reducing the financial burden on lower-income individuals. Third, those four Phase I UHC counties are also receiving support for primary care services through the provision of commodities and equipment.
Technical assistance to support RMNCAH services
The RMNCAH Technical Assistance Multi-Donor Trust Fund (MDTF), cofinanced by the U.S. Agency for International Development (USAID), the Department for International Development (DFID), and the Danish International Development Agency (Danida), complements the THS-UCP and the investment framework by providing technical assistance to enhance the effectiveness of Kenya’s national and county governments to achieve better and more sustainable RMNCAH results. Although the MDTF does not receive financial contributions from the GFF partnership, it represents an important collaboration and complementarity, since the MDTF objectives are directly aligned with the THS-UCP and provide key inputs to making the Investment Framework work at the county level.
Technical assistance has been provided in a number of areas that strengthen the health system, including: (1) for capacity building among national and county governments by standardizing counties’ planning and budgeting processes, which were highly fragmented; (2) for supply-chain management in 5 counties; (3) for coordinating stakeholders in 22 counties; (4) for RMNCAH-focused monitoring and evaluation in 8 counties; and (5) for mapping and tracking resources to ensure that all health investments (on-budget, off-budget, and in-kind) are reflected in the health sector’s annual work plan and that resources are linked with planning and reporting processes. More specifically, concerning area (5), the aim is to ensure that resources are linked with annual Medium-Term Expenditure Framework’s (MTEF’s) planning and annual sector reporting processes.
The MDTF has encouraged health leaders to share experiences and lessons learned, with the goal of working together in a more coordinated way, both among donors and within and across government sectors. It has also supported revisions of the tools government uses for performance review and planning and has helped develop a public financial management framework that allows county governments to “ring-fence” the funds allocated to health.
Results
In 2017, Kenya’s health system suffered a severe crisis in its health workforce that disrupted health system functioning for almost a year. Lengthy nationwide strikes by doctors and nurses impacted service delivery, as evidenced by sudden drops in the coverage of key services in 2017, as shown in this case study. Kenya’s recovery from this shock has been impressive: in the span of only one year (by 2018/19), the country has been able to achieve—and in many cases surpass—pre-strike levels of coverage that had been deteriorating since 2015.
Progress in mobilizing and using domestic resources for health at the county planning and budgeting level has also been observed. All 47 counties met the THS-UCP’s eligibility criteria of increased allocations to health in their budgets in the past two years, and some are allocating more than 30 percent of their budget to health (well above the 20 percent requirement). Six counties increased their budgets by more than 10 percent, 13 counties increased them by 5–10 percent, 26 counties increased them by less than 5 percent, and two counties kept their budgets constant (Figure 1). Of the remaining two counties, only Meru County declined significantly, dropping from 32 to 28 percent; the budget of the other county declined by just 1 percentage point.
Counties are also working to eliminate delays and improve the flow of funding, especially from the county revenue fund to the special purpose account, a ring-fenced account for conditional donor grants for health. On average, between 43 and 46 of the 47 counties transfer funds within 15 working days, a significant improvement from conditions before reform, when transfers of funding to and within counties and facilities could take 3 to 12 months due to a lack of clear mechanisms on how those funds should flow.
In summary, the introduction of high-impact, cost-effective RMNCAH interventions, the promotion of joint learning, and the monitoring of progress toward the core health goals have helped Kenya make measurable progress in its four focus indicators of antenatal care, skilled birth attendance, immunization, and family planning (Figure 2).
Figure 2
Percent of population in Kenya receiving antenatal care, immunizations, and family planning services, annually,
2015–2018
Increases in antenatal care, family planning, and child immunizations took place in Kenya from 2015 to 2018, including an impressive recovery in
2018 from severe health service disruptions that occurred in 2017
Women’s antenatal care (ANC) visits increased significantly between 2015 and 2018. In 2018, 48.6 percent of pregnant women attended at least four ANC (ANC4) visits, a 9.5 percentage-point increase over 2015 (Figure 3). Despite these increases, Figure 3 also highlights wide variations across counties, with 19 counties showing increases of 10 to 43 percentage points and 11 counties showing little or no progress (increases of less than 5 percentage points). The percentage of deliveries by skilled birth attendants also rose between 2015 and 2018, from 56.9 to 65.0 percent.
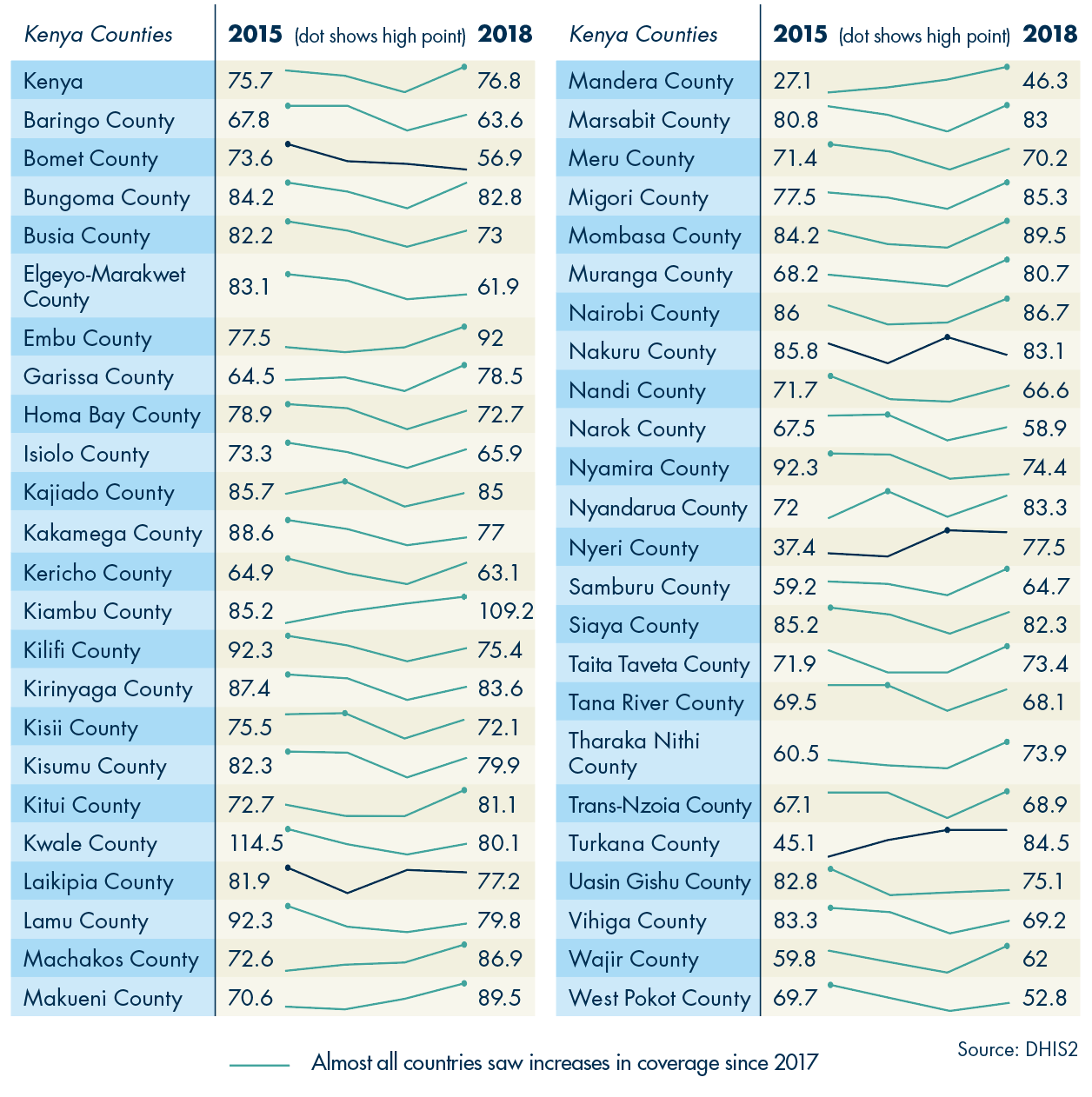
The proportion of children in Kenya under the age of one who were fully immunized remained almost flat between 2015 and 2018, rising slightly from 75.1 to 75.5 percent. It is important to note, however, that this indicator showed a strong rebound after the strikes, rising from 63.8 percent in 2017 to 75.5 percent in 2018. As with ANC4 coverage, progress varied widely across counties, with 20 counties experiencing increases and 27 experiencing declines in immunization rates (Figure 4). Large increases were seen in a few counties: Nyeri County saw the largest increase, rising from 37.4 percent in 2015 to 77.5 percent in 2018, a 40.1 percentage-point increase. Turkana County experienced the next-highest increase, rising from 45.1 percent in 2015 to 84.5 percent in 2018, a 39.4 percentage-point rise. Increases ranged from 2 to 19 percentage points in 15 countries and were less than 2 percentage points in 3 counties. Twenty-seven counties experienced declines, with immunization rates in 5 counties falling by less than 2 percentage points and rates in the other 22 counties falling by more than 2 percentage points. The decline in the rate of immunization was steepest in Kwale County, where it fell 34.4 percentage points.
The percentage of women of reproductive age who received modern family planning commodities dropped between 2015 and 2017, from 47.8 to 36.3 percent in 2017, a decline that is believed to be driven by the strike by doctors and nurses in 2017. Use of family planning services rose in 2018, reaching 44.1 percent, but did not fully recover to pre-strike levels. To further promote the increase of availability and use of family planning services, the THS-UCP project recently spent US$7 million on family planning commodities, with the objective of increasing supply and access. Nevertheless, an ongoing funding gap for procurement of family planning commodities could hamper progress.
Conclusion
Overall, Kenya has improved the coverage of key maternal and child health services such as antenatal care, skilled birth attendance, and family planning. The disruptions to the health system due to long-term nurse and doctor strikes, however, are not to be underestimated. Their impact is reflected in the mixed progress across indicators (child immunization, for example) and regions. Continuing to support and strengthen county-level shifts in planning, budgeting, and data use will be critical in identifying and addressing bottlenecks to achieve the goals of the KHSSP, with specific action plans that are tailored and responsive to the particular needs of each county.